- What are flu vaccines?
- What are the components in a flu vaccine?
- How many strains does a flu vaccine target?
- How does a flu vaccine work?
- Who decides flu vaccine strains each year?
- Why do we need a flu shot every year? What are the benefits?
- Is the yearly flu vaccine the same everywhere?
- How effective is the yearly flu vaccine?
- Is the flu vaccine still effective if it doesn’t match the circulating virus?
- Why do people skip the flu shot?
- Are flu shots safe? What are the possible adverse effects?
- Who should NOT get a flu vaccine?
- Who should delay vaccination or consult a healthcare professional?
- What are the alternatives to the traditional flu shot?
- What should I avoid after getting the flu shot?
- Why does flu vaccination work well for young children, even though their natural immunity is still developing?
1. What are flu vaccines?
Flu vaccines are medical preparations designed to protect against infection by influenza viruses, they are updated yearly to match expected strains.
The types of Flu Vaccines include:
- Inactivated (IIV) – contains killed flu viruses
- Live Attenuated (LAIV) – contains weakened live viruses
- Recombinant – made using genetic technology, no live virus.
Each type is designed for different age groups and health needs.
In short: Flu vaccines are safe and effective. They help your body recognize and fight flu viruses, reducing illness, hospitalizations, and deaths every season.

2. What are the components in a flu vaccine?
The ingredients in flu vaccines vary depending on the manufacturing technology and brand. Components are included to stimulate an immune response and ensure the vaccine’s safety and stability. Common components include:
∗∗Active Antigen Components
Trigger the immune system to produce antibodies that prevent the virus from entering cells.
∗∗Common Inactive but Necessary Additives
- Stabilizers: Prevent antigens from degrading during storage or transport.
- Antibiotics (trace amounts): Prevent bacterial contamination.
- Buffers and salts: Maintain proper pH and vaccine stability.
- Adjuvants (used in some older‑adult vaccines): Enhance the immune response.
- Preservatives: Prevent contamination, especially in multi‑dose vials.
- Trace residuals: Tiny amounts of substances that may remain from the manufacturing process.
All ingredients have specific purposes and are tested for safety. If you have allergies or other concerns, consult a healthcare professional.
3. How many strains does a flu vaccine target?
Most flu vaccines are quadrivalent, meaning they protect against four strains:
- 2 influenza A strains (H1N1 and H3N2)
- 2 influenza B strains (Victoria and Yamagata lineages)
Some older or specialized vaccines are trivalent (3 strains), but quadrivalent is now standard.
Timing: Get vaccinated by end of October in the Northern Hemisphere, the protection will last about 6 months, covering the peak flu season.
4. How does a flu vaccine work?
The flu vaccine trains your immune system by exposing it to harmless parts of the virus, so it can respond quickly if you encounter the real flu. After vaccination, your immune system:
- Produces antibodies (mainly against hemagglutinin)
- Activates T-cells and B-cells that remember the virus
This immunity helps prevent infection and reduces illness severity. Because flu viruses change every year, annual vaccination is recommended.
By getting vaccinated, you not only protect yourself but also help reduce the spread of flu in your community, especially to vulnerable people like the elderly, young children, and those with chronic health conditions ( known as herd immunity).
5. Who decides flu vaccine strains each year?
The selection of flu vaccine strains each year is a highly coordinated global public health process:
- The WHO, through the Global Influenza Surveillance and Response System (GISRS), collects influenza virus data from over 100 countries.
- The WHO holds two meetings each year, bringing together more than a hundred experts worldwide to review global trends and recommend four vaccine strains (2 influenza A + 2 influenza B).
- National regulatory agencies, such as the U.S. FDA, the European EMA, and China’s NMPA, approve the local vaccine composition based on WHO’s recommendations.
- Vaccine manufacturers then produce vaccines using the approved strains to ensure supply before the autumn vaccination season.
6. Why do we need a flu shot every year? What are the benefits?
- Keeps up with yearly mutations: The vaccine is updated each year to match the newest circulating strains.
- Reduces severe illness and death: Lowers the risk of hospitalization, pneumonia, and other complications; infections are usually milder.
- Lowers transmission: Reduces viral load, making you less likely to spread the flu to others.
- Protects high‑risk groups: Especially important for older adults, pregnant women, people with chronic conditions, and infants who can’t be vaccinated (herd immunity).
- Save time and costs: Prevents missed work or school and reduces healthcare expenses.
- Build community immunity: Widespread vaccination helps reduce overall flu activity.

7. Is the yearly flu vaccine the same everywhere?
No, flu vaccines are not exactly the same everywhere. Most countries follow WHO’s yearly recommendations, but final formulations can differ slightly due to:
- WHO strain updates: WHO recommends strains twice a year for the Northern and Southern Hemispheres.
- Local regulatory decisions: Agencies like the FDA, EMA, and NMPA usually follow WHO guidance, with only minor regional adjustments.
- Vaccine types and production methods: Countries may use trivalent or quadrivalent vaccines, and production may be egg‑based, cell‑based, or recombinant. Egg‑based methods can occasionally introduce small HA mutations too.
Global surveillance and vaccine‑effectiveness monitoring help ensure each region’s vaccine matches circulating flu strains as closely as possible.
8. How effective is the yearly flu vaccine?
The effectiveness of the annual flu vaccine depends on factors such as strain match, age, health status, and the types of viruses circulating that season:
∗∗Preventing symptomatic infection
- 40~60% effective when strains match well.
- 20~30% or lower when the match is poor due to viral changes or egg‑adapted mutations.
∗∗Preventing severe illness (even if infected)
- Reduces hospitalization risk by 40~80%.
- Lowers children’s ICU admission risk by up to 74%.
- Significantly reduces flu‑related deaths in older adults and people with chronic diseases.
∗∗Benefits even with low match
- Helps reduce severity, shorten illness, and ease pressure on healthcare systems.
- High‑dose or adjuvanted vaccines are recommended for older adults.
Overall, yearly flu vaccination remains one of the most effective ways to prevent influenza and its serious complications.

9. Is the flu vaccine still effective if it doesn’t match the circulating virus?
Yes, a mismatched vaccine may offer less protection against mild illness from flu, but it still plays a key role in preventing severe outcomes.
- Reduces serious risks: Even in poorly matched seasons, vaccines significantly lower hospitalization and death rates, preventing millions of infections and thousands of severe cases.
- Partial protection: Cross-reactive immunity helps your body recognize shared virus components, reducing symptom severity and speeding recovery.
That’s why health authorities recommend annual vaccination, even when the match isn’t perfect.
10. Why do people skip the flu shot?
Despite strong recommendations, flu vaccination rates remain low. Common reasons include:
- Myths and misinformation
- Distrust of health authorities or pharma companies
- Low perceived risk (“Flu is mild”)
- Access issues: cost, location, and timing
- Personal beliefs: “natural immunity,” autonomy, or rare religious reasons
- Past experiences: bad reaction or illness blamed on vaccine
- Confusion about annual shots: viruses mutate, or immunity fades
- Social influence: friends, family, and social media spreading false information
11. Are flu shots safe? What are the possible adverse effects?
The flu vaccine is very safe, with hundreds of millions of doses given each year and extremely rare serious side effects. For most people, the risks from flu infection are far greater than the risks from the vaccine.
Common mild reactions (resolve in 1~2 days)
- Soreness or redness at the injection site
- Mild fever, headache, fatigue, or muscle aches
- Occasional brief fainting in teens (rest 15 minutes after vaccination)
Rare but important reactions
- Allergic reactions: Trouble breathing, hives, or facial swelling, usually within minutes to hours, treatable on site.
- Guillain–Barré Syndrome (GBS): About 1~2 cases per million doses; the risk is higher after influenza infection itself.
Special note: Most people with egg allergies can still safely get the flu vaccine. Only those with a severe allergy to vaccine components should avoid it.
12. Who should NOT get a flu vaccine?
While flu shots are safe for most people aged 6 months and older, some should avoid them or consult a doctor first:
- Infants under 6 months
- People with severe, life-threatening allergy to any vaccine ingredient (gelatin or antibiotics), excluding egg proteins.
- Anyone who had a severe allergic reaction to a previous flu vaccine or a specific ingredient.
There are different types of flu vaccines such as inactivated, recombinant, and live attenuated nasal spray, the contraindications may vary by formulations. Always consult a healthcare provider if you have concerns about allergies, medical history, or vaccine suitability.
13. Who should delay vaccination or consult a healthcare professional?
Most people can safely receive the flu vaccine, but vaccination should be postponed or discussed with a healthcare professional if you have any of below:
- Fever (≥38°C) or a moderate/severe acute illness: Wait until symptoms improve.
- A history of Guillain–Barré syndrome (GBS): Especially if it occurred within 6 weeks of a previous flu shot, consult a doctor.
- A severe allergic reaction to a flu vaccine or its components: Do not receive the same type again; seek advice from an allergy specialist.
Notes: People with mild allergies such as egg allergy, pregnant individuals, those with chronic diseases, or those with weakened immunity can safely receive the vaccine and are priority groups (use inactivated or recombinant vaccines; avoid live nasal spray vaccines).
If unsure about your suitability, refer to guidances from CDC, WHO, or local health authorities, or consult a doctor.
14. What are the alternatives to the traditional flu shot?
Besides the standard injectable flu vaccine, other options exist, though availability varies by country:
- High‑dose vaccine: For adults ≥65 to boost immune response.
- Adjuvanted vaccine: Also mainly for those ≥65 to enhance immunity.
- Recombinant vaccine: Egg‑free, virus‑free; usually for adults ≥18.
- Cell‑based vaccine: Produced without eggs; suitable for people with egg allergy (age range depends on local approval).
- LAIV nasal spray: Allowed in some countries for healthy, non‑pregnant people aged 2~49; not for immunocompromised individuals, pregnant women, asthma patients, or children/teens on aspirin.
- Needle‑free injectors: Available in limited regions for ages 18~64; not a routine option.
Note: Standard inactivated vaccines remain the primary choice in most places, while alternatives may be limited to specific groups or require out‑of‑pocket payment.
15. What should I avoid after getting the flu shot?
After getting a flu shot, most people don’t need to change their routine significantly, just listen to your body and give it a little extra care for a day or two.
- Don’t rub the injection site; keep it clean.
- Skip heavy workouts for a day if you feel unwell.
- Avoid heavy drinking for 1~2 days.
- Don’t take painkillers unless needed.
- Avoid close contact with sick people (vaccine takes about 2 weeks to work).
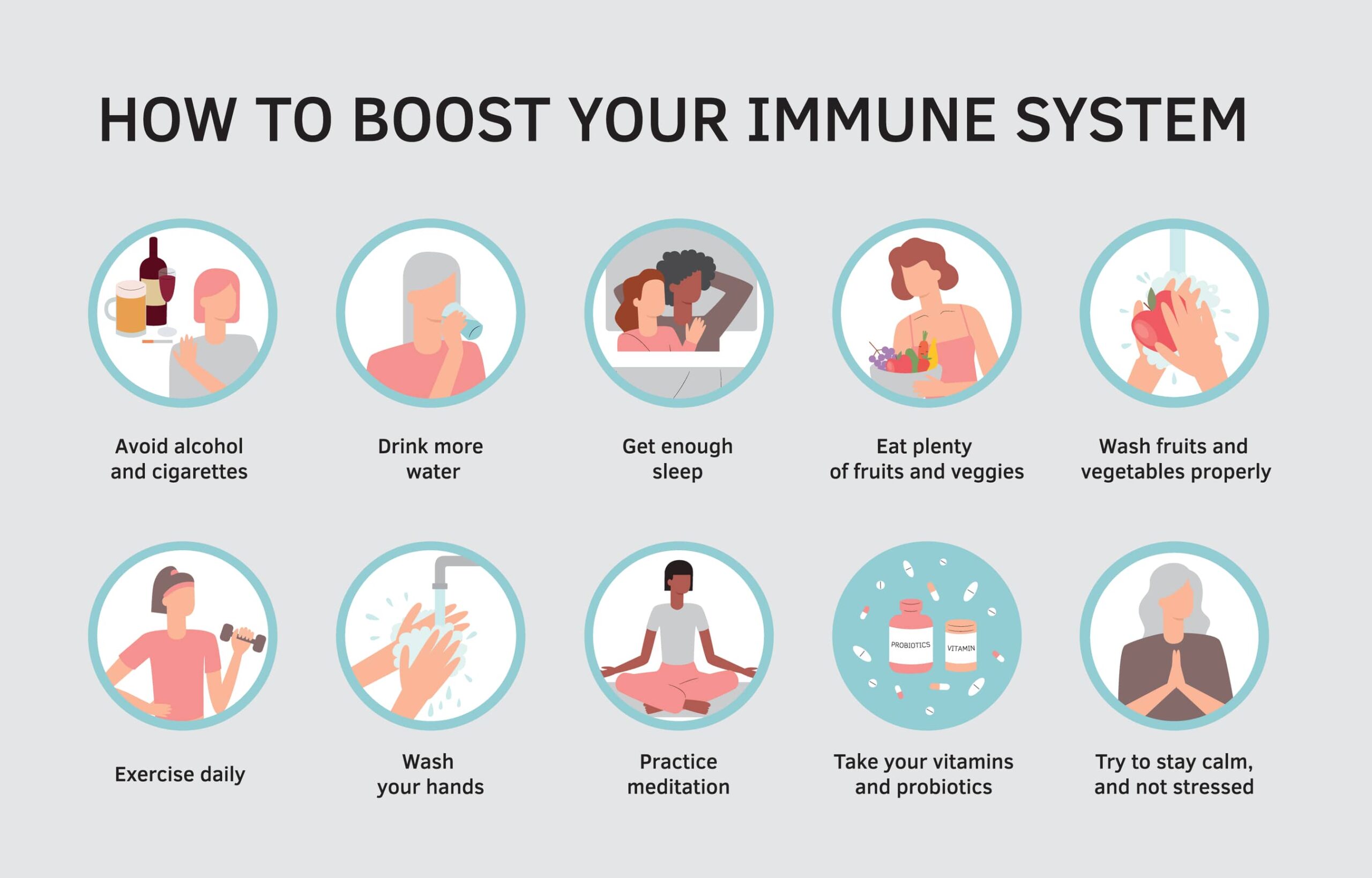
How to boost your immune system during flu season
16. Why does flu vaccination work well for young children, even though their natural immunity is still developing?
Young children have no prior exposure to influenza viruses and therefore lack strain‑specific antibodies and immune memory. This makes them highly vulnerable to infection, and children under two years face higher risks of severe complications such as pneumonia, ear infections, and hospitalization.
The flu vaccine safely activates a child’s immune system and helps build antibodies and immune memory. Although their immune response is still developing, most children gain good protection when vaccinated as recommended (first‑time recipients aged 6 months to 8 years need two doses at least 4 weeks apart).
Vaccinating children also reduces virus spread in households and childcare settings, offering indirect protection to infants under 6 months, who cannot be vaccinated but are at highest risk.
For these reasons, global health authorities recommend that all children aged 6 months and older receive the flu vaccine every year.