Diabetes Mellitus : Definition
Western Medicine
Pancreatic Structure
Pancreas
Ampulla of Vater Duodenum
Diabetes is a disease that is becoming increasingly common and progressively complicated. There were approximately 175 million people afflicted with diabetes worldwide, according to a 1994 report released during the 15th International Diabetes Federation Congress. Clinicians used to treat it as a disease of high blood glucose; however, we now view it as a disease of many factors, involving abnormal breakdown of fat, protein and glucose. Glucose is the sugar our body uses as energy for our cells. Current management involves controlling glucose levels to minimize complications in the finer blood vessels (microvasculature) as well as controlling other metabolic abnormalities such as high blood pressure, high cholesterol / triglycerides, or obesity to prevent complications in the bigger blood vessels (macrovasculature).
Diabetes mellitus is a term that was coined by Aretaeus the Cappadocian, a first century Greek physician. According to the physician, "diabetes" means "to flow through like a siphon", and "mellitus" meant "honey". He also described diabetes as a disease that led to "sweet urine" and "siphoning or melting down of the flesh and limbs into urine".
The definition and management of diabetes mellitus have changed over the years. We used to differentiate the two different types of diabetes by its time of onset. A patient was diagnosed with juvenile-onset diabetes if he was discovered to have high blood glucose during childhood. The patient would be diagnosed with adult-onset diabetes if he was discovered to have uncontrolled glucose during adulthood, usually when they were elderly.
However, there were many patients who fell in between the age groups. In the last decade, there has been a dramatic increase of diabetes among people in their 20s and 30s; therefore, the terms "juvenile-onset" and "adult-onset" diabetes have become obsolete.
Patients were also categorized into having "insulin dependent diabetes mellitus (IDDM)" or "non-insulin dependent diabetes mellitus (NIDDM)". However, there are many patients now receiving both oral medications as well as insulins in order to control their diabetes.
Individuals with diabetes are currently categorized has being Type 1or Type 2.
Type 1 diabetes results from an absolute lack of insulin.
Type 2 diabetes is due to a relative lack of insulin or insensitivity to the available insulin.
There are also other intermediate stages of the disease:.
Gestational diabetes occurs when a woman develops glucose intolerance only during pregnancy (this means her glucose levels rise higher due to physiological stress and the body is unable to secrete enough insulin to drive the glucose into the body's cells in order to utilize the glucose.) This is usually detected during or after the 2nd trimester and the woman carries a higher risk of developing diabetes later on in life.
Impaired glucose intolerance (IGT) or impaired fasting glucose (IFG), occurs when blood glucose is higher than normal, but not high enough to be classified as diabetes. Patients with IGT or IFG who continue to have uncontrolled glucose levels may eventually develop type 2 diabetes within 10 years.
Many view diabetes as a progressive disease that initially surfaces as impaired glucose intolerance with a high post-meal glucose. (This means the glucose level is abnormally high after eating a meal.) The high glucose levels continue to demand the pancreas to secrete more insulin resulting in a state of hyperinsulinemia. However, the body becomes resistant to the insulin, and later develops a relative lack of insulin, and high fasting (before eating) glucose levels. Typically this pattern presents itself as type 2 diabetes. Eventual exhaustion of the islet cells (a type of cell in the pancreas that makes insulin) leads to a final stage of definite or absolute lack of insulin with a typical presentation of type 1 diabetes.
Metabolic Defects in Type 2 Diabetes
Within a population, type 2 diabetes is much more common than type 1 diabetes. For example, there are approximately 16 million people afflicted with diabetes in the United States, with approximately 90 to 95% of the patients having type 2 disease while only 5 to 10% has type 1 disease. Epidemiological studies have also found that type 2 disease is more common among African-Americans, Hispanic-Americans, Native Americans, Asian-Americans, and Pacific Islanders. These ethinic populations are more at risk of developing diabetes probably due to a genetic predisposition as well as the rapid adaptations to western cultures that include high fat diet and sedentary lifestyles.
Chinese Medicine
Huang Di Hei Jing (The Yellow Emperor's classic of Internal Medicine) is the earliest TCM theoretic book. It is divided into two parts Suwen (The Book of plain Questions) and Lingshu (The Book of Miraculous Pivot)
In ancient China, the word "diabetes" did not exist. However, an early definition of the illness can be found in the medical classic Huang Di Nei Jing (The Yellow Emperor's Classic of Internal Medicine) written during the Han Dynasty (approx. 200 BC). Under this book's Suwen (The Book of Plain Questions) section, diabetes was defined by the following symptoms "xiao ke" and "fei xiao," which translate into excessive drinking, and "ge xiao" and "xiao zhong," which mean excessive eating. According to the Suwen, additional clues to the disease include excreting large amounts of urine with sugar in it and weight loss. The ancient Chinese people also thought it was caused by improper diet and mainly affected the upper class. The Book of Plain Questions describes the diabetes sufferer as follows: " When, a person has eaten too much greasy and sweet food, the body produces dry-heat evils which causes qi to stay in the middle-burner of the body until finally the qi flows upward and spills over resulting in diabetes." The "Efficacious Formulae Recorded from Antiquity to the Present," penned by medical practitioner Zhen, Li-yan during the Sui Dynasty (589~618 AD), wrote that diabetes patients usually suffer from the following symptoms: "Frequent thirst that leads to excessive drinking, excessive urination, and urine that is sweet and without fat."
Diabetes is generally attributed to a deficiency of body fluids and the excessive accumulation of dry or heat evils inside the body. Dry and heat evils come from external environmental sources such as an improper diet and are transformed internally into disease causing factors such as a kidney yin deficiency. Dry and heat evils trigger certain organs in the body to react negatively. The organs that are most affected are the lung, stomach and kidney.
The Lungs: The lungs are responsible for the transformation and movement of water in the body. Dry-heat hurts the lungs and causes body fluid to flow straight down freely without being distributed to the rest of the body. This results in frequency in urination, thirst and excessive drinking, which are all symptoms of diabetes.
The Stomach: The stomach is a reservoir for food and drink. An intense stomach fire is caused by dry-heat which damages the stomach. As a result, the metabolic rate rises and triggers an increase in appetite and constipation. An increase in appetite is also another hallmark symptom of diabetes.
The Kidneys: Since the kidneys control water metabolism, deficiency of the kidney-yin and "virtual fire"(the heat developed inside the body by a relative excess of yang) creates dry and heat evils. This damages the "vaporization" function and results in the kidneys' failure to separate turbid water, which will be turned into urine and clean water, which is reused by the body. It also affects the opening and closing of the bladder. The end result is an excessive amount of urine, urinary frequency and the production of urine with traces of sugar.
Understanding water metabolism from a TCM perspective
In western medicine diabetes mellitus is a metabolic disorder that occurs when there is a chronically high level of glucose (sugar) in the blood caused by a deficiency or complete lack of insulin. The insulin deficiency and high glucose levels cause serious damage to the body over time if left untreated and in severe cases may cause death.
This western understanding of diabetes is not present in TCM. Its diagnosis is based on the clinical symptoms of diabetes such as excessive thirst, hunger and urination, which may or may not be accompanied by sudden weight loss. Depending on each individual's symptoms, it is further classified into four types of disharmony patterns discussed in the diagnosis section. Even though two people may be diagnosed with diabetes from a western perspective, these individuals may present with two different disharmony types from a TCM perspective and thus will be treated differently.
Diabetes Mellitus : Causes
Western Medicine
Higher than normal glucose levels are results of defective insulin secretion, insulin action or both. The pathology of type 1 disease involves islet cell destruction and beta-cell loss (two types of cells in the pancreas responsible for making and secreting insulin) leading to an absolute lack of insulin. It is believed that cytotoxic T lymphocytes and macrophages which are types of immune cells, target the destruction of islet cells possibly due to viral causes, toxins, or autoimmune stimulation.
In contrast, the size and number of beta cells are relatively normal in type 2 disease. The number of beta cells may even be increased due to a compensatory mechanism of the pancreas to secrete more insulin as a response to a state of insulin resistance. In addition, the liver of a patient with type 2 diabetes may be producing too much glucose or the timing of insulin secretion is inappropriate.
Chinese Medicine
The primary causes of diabetes are detailed below.
| 1. | Congenital Deficiency |
| Individuals born with a congenital deficiency are genetically susceptible to this disease. Dysfunction of the lungs and kidneys affects the water metabolism in the same way dysfunction of the spleen and stomach affects digestive power. In turn, these organs cannot function properly and diabetes is caused by the mechanisms listed in the definition section. | |
| 2. | Improper Diet |
| Over consumption of greasy food and alcohol drinks may impair the stomach and the spleen, which in turn fail to transform and transport these substances into nutrition for the body. The undigested food then accumulates and transforms into heat and dryness evils, and consumes the body fluid, which causes thirst and excessive drinking. | |
| 3. | Emotional Disorders |
| Over stimulation of emotions may spark stagnation of vital qi and then transform it into a heat-evil, which consumes the yin-fluid of organs like the lungs and stomach. Symptoms of diabetes occur when the body's metabolism becomes unbalanced from dysfunction of the lungs and spleen. | |
| 4. | Tension |
| Overwork leads to consumption of yin-essence in the kidneys and produces internal fire or heat evils. This accelerates the depletion the nutrients and triggers a rise in metabolic rates, which results in increased appetite but with weight loss. An increased appetite and weight loss are some of the classic symptoms of diabetes. | |
| 5. | Pleasure Indulgences |
| Excessive sexual activity can cause consumption of kidney essence (a yin-component that includes sperm and egg cells and blood), which leads to a relative excess of yang. When this occurs, a "virtual fire" or a heat evil is created which heats up the lungs and stomach causing organ damage. In turn, these organs cannot function properly and diabetes is caused by the mechanisms listed in the definition section. | |
| 6. | Drugs |
| Improperly used libido drugs can cause heat evils to accumulate in the lower-burner. When individuals consume them for a long time and get older, the kidney yin will become insufficient and cause damage to the kidneys' "vaporization" function. See definition section. The damage of this function is one of the causes of diabetes. |
Diabetes Mellitus : Symptoms
Western Medicine
1. Type 1 Diabetes:
The most typical symptoms of diabetes or high blood glucose include frequent urination, frequent thirst, and frequent hunger or eating. These are usually more common in type 1 patients. Other characteristics that are more typical of type 1 patients include:
younger age of onset
human leukocyte antigen (HLA) or genetic predisposition
presence of islet-cell antibody
fatigue
thin appearance
prone to ketosis (an acute situation when the body starts to break down fat and produces ketone bodies due to an absolute lack of insulin and extremely high level of glucose)
high glucose levels (hyperglycemia) or low glucose levels (hypoglycemia)
absolute dependence on insulin that must be injected into the body
2. Type 2 Diabetes
Because type 2 patients only have a relative deficiency of insulin, most symptoms are not as pronounced, and usually occur later in life. Type 2 patients are less likely to be ketotic (see above), with only a third of them needing insulin injections. In addition, they are often overweight, have abnormal blood pressure and fat levels measured as cholesterol / triglycerides and have frequent vascular or neurologic complications. See below.
3. When diabetes is uncontrolled
Uncontrolled diabetes occurs when glucose levels remain persistently high and is typically associated with long-term complications. It is proposed that the persistent hyperglycemia (high glucose levels) and the formation of glycated proteins (including glycosylated hemoglobin, HbA1c) are responsible for weakening the capillary walls and clogging the small blood vessels. As a result, the microvascular complications such as retinopathy (damage to the eyes), nephropathy (damage to the kidney), and neuropathy (damage to the nerves) occur.
Diabetic retinopathy is the leading cause of blindness in the United States, and is preceded by microaneurisms (focal dilation of retinal capillaries occurring in diabetes), hemorrhages, edema (swelling), fibrosis (scarring), and retinal detachment.
Diabetic nephropathy is the leading cause of end stage kidney disease (ESRD) in the United States. It is preceded by presence of protein in the urine, abnormal kidney function and increased blood pressure.
Neuropathy can present itself in two forms: peripheral or autonomic neuropathy. Symptoms of peripheral neuropathy include tingling, numbness, or burning of extremities as well as abnormal vibratory, sensory, and reflexes mostly in the lower extremities. Diabetic neuropathy is the most common cause of non-traumatic amputations in the United States. The other form of neuropathy is autonomic, in which patients may have problems with digestion and, impotence or suffer from improper cardiovascular reflexes.
Furthermore, uncontrolled diabetes can also lead to macrovascular complications such as coronary heart diseases and peripheral artery disease that presents with heart problems, pain upon walking and inability to walk far. In summary, diabetes can be a devastating disease causing harmful effects to the eyes, kidney, nerves, genitals, and heart.
Chinese Medicine
TCM practitioners recognize symptoms of diabetes from both a western and eastern point of view.
Clinical distinction in western medicine: Type I diabetes occurs in individuals who do not produce any insulin. The onset of Type I diabetes begins at a young age. Clinical symptoms change quickly and become increasingly more serious. Typical signs include excessive and constant thirst, excessive drinking and eating, excreting an excessive amount of urine with sugar in it, and weight loss.
Type II diabetes occurs in individuals who do not have enough insulin or whose insulin does not work properly. The onset of Type II diabetes usually begins in middle or old age. However, the disease may be present in a sub clinical form for years before diagnosis. The main symptoms are extreme fatigue, dry mouth and excessive thirst. Other symptoms like excessive urination, and excessive eating may not be as obvious with this type.
According to Traditional Chinese Medicine diagnosis, the disease can be divided into four types of disharmony patterns:
| 1. | Yin Deficiency and Excessive Heat Type Symptoms related to this type include thirst for cold drinks, an increased appetite, and dislike of heat and emotional imbalances. Other symptoms include dark urine, constipation, an appearance of a red tongue with a yellow coating and a pulse that feels rapid and taut or slippery. |
| 2. | Deficiency of Qi and Yin Type Symptoms include shortness of breath, heart palpitations, fatigue and weakness that can lead to reluctance to speak. Additional symptoms include: constant thirst, spontaneous sweating, sweating during sleep, being easily irritable, having trouble sleeping, feeling heat in the palms of the hands and soles of the feet, dark urine and constipation. The tongue appears dry, red and swollen, while the coating is scaled off. The pulse is weak and uneven. |
| 3. | Blood Stasis and Internal Obstructed Type Symptoms include darkened skin, weight loss and malaise, fullness and blurred pain in the chest, numbness or stabbing pain in limbs, which worsens at night. People who suffer from this form of diabetes will also have purple-colored lips, and a tongue that is dark in color or appears bruised. The tongue will also be covered with a thin white or yellow colored coating, or appear dark and bruised. The pulse feels taut or uneven. |
| 4. | Deficiency of Yin and YangType Symptoms include a below normal body temperature, aversion to coldness with cold feeling limbs, a pale face, ringing in the ears, weakness in the lower back, occasional fever, sweating at night, impotence or premature ejaculation of sperm. The stool is loose and excessive clear urine is passed. The bulging tongue appears light pink, and is blanketed with a thin white coating or a white greasy fur. The pulse is faint or rapid and uneven. |
Other related patterns:
Accumulated Internal Wet Heat Type: The body appears fat and bloated. The mouth is dry and has a bitter taste with foul smelling burps. Other symptoms include itchy skin, yellow and cloudy urine, and loose stool. The tongue appears swollen and is covered with a yellow greasy or turbid yellow greasy fur coating. The pulse feels weak and slippery.
Diabetes Mellitus : Diagnosis
Western Medicine
There are various methods to evaluate and diagnose diabetes: detection of typical symptoms such as random glucose level, fasting glucose, two-hour post-load glucose level, and HbA1c (an indicator of glycemic (glucose) control over a 3-4 month period). According to the 1985 World Health Organization (WHO) report, diabetes is defined by:
A fasting plasma glucose (FPG) of 140 mg/dl (7.8 mmol/l) or greater
A 2-hour plasma glucose (2-h PG) post 75-gm of oral glucose tolerance test (OGTT) level of 200 mg/dl (11.1 mmol/l)
Both of the above
However, the latest American Diabetes Association (ADA) expert committee finds that there is a greater degree of hyperglycemia amongst patients who have FPG of 140 mg/dl or higher than those who have 2-h PG of 200 mg/dl or higher. Almost all patients with FPG 140 mg/dl or higher have 2-h PG levels of 200 mg/dl or higher. However, not all patients with 2-h PG of 200 mg/dl or higher have FPG of 140 mg/dl or higher. Therefore, the ADA currently recommends the diagnosis of diabetes be based on a lower level of FPG.
A patient is diagnosed with diabetes if he has typical hyperglycemic symptoms with a random plasma glucose of 200 mg/dl (11.1 mmol/l) or greater, confirmed on a subsequent day by one of the following criteria:
Typical symptoms of diabetes plus a random plasma glucose of 200 mg/dl (11.1 mmol/l)
A fasting (at least 8 hours of no caloric intake) plasma glucose of 126 mg/dl (7 mmol/l) instead of 140 mg/dl
A 2-hour post load glucose level of > 200 mg/dl (11.1 mmol/l) after a 75-gram anhydrous glucose load.
Chinese Medicine
TCM practitioners will diagnosis diabetes according to its clinical symptoms and further characterize it by the disharmony pattern an individual displays.
Diabetes, as is commonly understood from a western medicine perspective, is largely dependent on western methodologies for diagnosis. (See western medicine diagnosis section.)
TCM Examination Techniques:
Diagnosis in TCM is based on four examination techniques. The first is "questioning." The TCM practitioner will want to know what the individual's current complaints are, and their family's medical history. The second technique is "observation." Physical features of the body such as the face, tongue, hair, nails, sputum (mucus that is coughed up) and examining the area of pain all offer clues to the problem. The tongue is particularly useful gage to assess illness because it is seen as a window to look at the functioning of internal organs. The third technique is "hearing and smelling." Smelling the sputum and breath and listening to the sounds coming from the chest offer additional clues. The last technique used in examination is "touching." Feeling the pulse is a cornerstone of TCM diagnosis and gives the TCM practitioner a lot of information about the body's imbalance.
In TCM theory, diabetes is characterized by a combination of symptoms below:
Excessive eating
Excessive drinking
Excessive urine
Wasting of body tissues or weight loss
Note: If a TCM practitioner suspects there might be a serious problem that Chinese medicine alone cannot treat, he or she will recommend the individual see a western doctor for further follow up. When an individual experiences severe symptoms like those listed above, it should be taken very seriously, and the appropriate medical care should be sought out preferably in an emergency setting.
The four Types of Disharmony Patterns Even though diabetes can be diagnosed from the above symptoms, the information gathered from the TCM physical examination is used to determine which type of disharmony pattern an individual has. This is important because at the various stages of a disease, a varicty of disharmony patterns are present which require different types of therapy. This is the reason two individuals with the same disease may be treated very differently by their TCM practitioner.
| 1. | Yin Deficiency and Heat Excessive Type |
| In TCM, yin deficiencycommonly refers to a deficiency of yin fluids such as blood and body fluids. Without sufficient nourishment by these fluids, excitatory functions (heat excessive manifestations) become dominant and lead to symptoms of fever, thirst or increased appetite. | |
| 2. | Deficiency of Qi and Yin Type |
| Qi can be interpreted as the "life energy" or "life force," that flows within us. Deficiencies in qi and yin result in organ dysfunction. In diabetes, the most affected organs are the lungs, stomach and kidneys. | |
| 3. | Blood Stasis and Internal Obstructed Type |
| This refers to a state where theblood cannot circulate smoothly, and is usually accompanied by qi stagnation. The organs lose nutrients from the blood, which cause symptoms like numbness in the limbs or localized tissue death. For example, people with diabetes may suffer from ulcerations in their legs and feet due to poor blood supply. | |
| 4. | Deficiency of Yin and Yang Type |
| The body's physiological functions (yang) and physical forms (yin) are maintained in constant balance to achieve health. When vital qi is severely deficient for a long time, this type will develop. It is a more general type of deficiency that can occur in many diseases such as diabetes. |
Other Related Disharmony Patterns: Accumulated Internal Wet Heat Type Improper diet is one of the causes of diabetes from a TCM perspective. This impairs the proper functioning of the spleen and stomach, which leads to formation of wet and heat evils. These evils affect the fluid metabolism inside the body, and diabetes symptoms like excessive thirst and hunger can appear.
Diabetes should be differentiated from hyperthyroidism (over-functioning of the thyroid gland)
Sometimes it is difficult to distinguish diabetes from hyperthyroidism since both share similar symptoms. In both conditions there may be the presence of an increased appetite associated with weight loss. Diabetes patients are frequently thirsty, and excrete an excessive amount urine with glucose (sugar) present in it. However, people suffering from hyperthyroidism experience irritability, excrete loose yellow stools, and have eyelid retraction and eyeball protrusion. Individuals with this condition may also suffer from a rapid and forceful heartbeat, and swelling of the thyroid gland in the neck. To safely make the distinction, laboratory examinations of the blood and urine can be done to diagnose these two conditions.
Diabetes Mellitus : Treatment
Western Medicine
1. Pharmacological Therapy:
Type 1 Diabetes
Insulin is the mainstay therapy for patients with type 1 disease. Most patients are on human insulins, which are synthesized by recombinant DNA technology. Beef (no longer available in the U.S.) and pork insulins are less preferred due to potential of antigenic (allergic) reactions such as itching and skin reactions at the injection sites. Of the available insulins, some are rapid acting, or short acting, which are used mainly before each meal. Others are intermediate acting, or long acting, which are injected once or twice daily under the skin. Table 1 is a summary of the onsets of action, duration of action and other characteristics of the various insulins available (in the United States).
Click here to see the Table 1
Type 2 Diabetes
Of the proposed pathology of type 2 diabetes (see figure 1), there are now different oral pharmacological agents to target the specific defects: there are three categories of agents, the insulin secretagogues, inhibitors of glucose breakdown, and the insulin sensitizers. The insulin secretagogues include sulfonylureas and metiglinides, which are used to stimulate more insulin secretion. Alpha-glucosidase inhibitors delay the absorption of glucose and are usually used to control post-meal hyperglycemia. The insulin sensitizers include biguanides and thiazolidinediones, which can help the available insulin to be taken up more effectively. Table 2 lists the different agents with their sites and mechanisms of actions.
Click here to see the Table 2 Pharmacologic Classes to Control Hyperglycemia in Type 2 Diabetes
The selection of agents for a patient with type 2 disease will depend on the degree of hyperglycemia, particular defects, as well as other contraindications that may be present. Table 3 lists the agents according to their relative potency, other non-glycemic effects and adverse effects.
Click here to see the Table 3 Relative Efficacy and Adverse Effects of the Oral Agents Used in Type 2 Diabetes
If we look at the patient according to the natural progression of diabetes, oral agents can also be picked according to the severity of disease. (See table 2) For example, an alpha glucosidase inhibitor or metiglinide may be most appropriate for someone who has mildly elevated glucose level after eating a meal. As this patient becomes less controlled with higher glucose and elevated fasting levels, we may then consider sulfonylureas, biguanides, or thiazolidinediones, all of which are considered more potent agents. There will be patients who may have multiple defects in the pathogenesis of their disease, therefore, will require a combination of agents (with different mechanisms of action) in order to control their diabetes. This can include the combination of different oral agents as well as combination of oral agents and insulins. Metformin can be particularly useful among patients who have concurrent problems with weight, cholesterol and triglycerides because it can also improve these indices. Concerns with the use of these oral agents lie in the side effects they can cause. Therefore, frequent and regular monitoring of patients is necessary to avoid hypoglycemia while they are on sulfonylureas, and to avoid stomach gas and diarrhea while they are on metformin. Metformin is also associated with a rare problem of lactic acidosis when it's accumulated in the body with deterioration of kidney function. Gastrointestinal gas and diarrhea are often causes of therapy discontinuation in patients taking acarbose and miglitol. The thiazolidinediones are also associated with rare liver toxicities and need frequent monitoring of the liver enzymes.
2. Therapeutic Approach:
It's recommended that the first stage of therapy for diabetes should include diet and exercise. An average size adult patient with diabetes should receive approximately 2000 calories per day with 60% carbohydrate, 20% protein, and 20% fat. However, calories or fat should be more restricted if the patient is overweight or has abnormal cholesterol / triglycerides; carbohydrate limited if glucose is uncontrolled; and protein also restricted if the patient has kidney complications from diabetes. Exercise should be incorporated into the therapeutic program (with doctor's approval and supervision) because it will enhance the body's sensitivity to insulin and increase utilization of glucose. Diet and exercise should be encouraged in all patients with diabetes and should remain a component of the therapeutic program as long as patients are compliant and gain benefits. Unfortunately, there are many patients who are not willing to diet or physically unable to exercise, and therefore should receive medications to aggressively control glucose early on during their disease.
Type 1 Diabetes
In a patient with newly diagnosed type 1diabetes, clinicians often start with a simple schedule of insulins. To improve glucose control, doses of the insulin(s) and / or the schedule may have to be adjusted often and on an as-needed basis. A typical regimen to start with includes intermediate- or long-acting insulin once or twice daily with short- or rapid-acting insulin before meals. However, patients with type 1 disease often have big fluctuations of glucose levels and suffer from extreme hyperglycemia or hypoglycemia. Therefore, tighter control is often necessary. Until recently, changing the timing of insulin injections and the dosage of different insulins were all that could be done to maximize glycemic control in type 1 patients. Over the last two years, however, rapid acting insulins have been made available, which made the control of glucose more precise. (See table 1) Instead of injecting the short-acting regular insulin about 30 minutes before meals, patients can inject the new rapid-acting insulins (lispro, aspart) within 15 minutes before meals. In addition, the newly available basal insulin glargine will make the control of glucose more consistent due to its slow release profile, which acts similarly to the physiological pattern of insulin release in our body.
tap the syringe to rid it of any air bubbles.
Prick the skin and underlying  fatty tissue to avoid injecting into an artery or vein.
fatty tissue to avoid injecting into an artery or vein.
Type 2 Diabetes
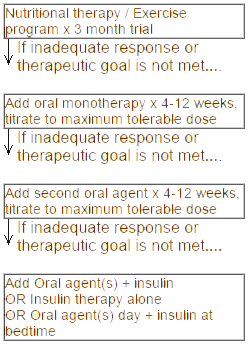
Due to the recent differentiation in the pathogenesis of type 2 diabetes, there have been changes in the way we manage the disease. As previously mentioned, type 1 patients have an absolute lack of insulin and require insulin injections; type 2 patients have a relative lack of insulin, either due to insensitivity to insulin or an insulin receptor defect, improper timing of insulin secretion, abnormal glucose production, or a combination of these factors. In patients with type 2 diabetes, herapeutic approaches should target the specific defect(s) in each patient. A proposed algorithm based on the level of glycemic control is described as following:
Chinese Medicine
Even in ancient times, TCM practitioners knew diabetes was a serious life threatening disease if not treated properly. Below lists some of the prescription examples used to treat the different disharmony patterns that occur in diabetes.
Yin Deficiency and Heat Excessive Type
Therapeutic aim: Clears away heat and dry evils, nourishes yin to promote the production of body fluid
Prescription:
Individuals with minor cases:
Xiaoke Fang
Huang lian
golden thread
Gau lou gen
snakegourd root
Sheng di huang zhi
juice of fresh rehmannia root
Hua fen
pollen
Ou zhi
Juice of fresh lotus root
Ren ru
human milk
Individuals with severe cases:
Wu zhi yu quan pill
Huang lian
golden thread
Zhi mu
common anemarrhena root
Wu mei
dark plum
Gan cai
liquorice root
Ren shen
ginseng
Mai dong
dwarf lilyturf tuber
Wu wi zi
Chinese magnolia vine fruit
Di huang
rehmannia root
Dang gui
Chinese angelica
Hua fen
pollen
Ge gen
kudzu vine root
Lian rou
lotus rhizome node
Ren ru
human milk
Niu ru
milk
Zhe zhi
juice of Sugar cane
Li zhi
pear juice
Ou zhi
juice of fresh lotus root
Deficiency of Qi and Yin Type
Therapeutic aim: Invigorates qi and nourishes yin
Prescription:
Individuals with minor cases:
Huang qi decoction
Huang qi
milkvetch root
Fu ling
Indian bread
Mai dong
dwarf lilyturf tuber
Di huang
rehmannia root
Tian hua fen
snakegourd root
Wu wi zi
Chinese magnolia vine fruit
Gan cao
liquorice root
Individuals with severe cases:
Di huang drink
Ren shen
ginseng
Huang qi
milkvetch root
Tian mai dong
cochin Chinese asparagus root
Shi hu
dendrobium
Pi pa ye
loquate leaf
Ze xie
oriental water plantain root
Zhi qiao
orange fruit
Sheng shu di
rehmannia root (processed & unprocessed)
Blood Stasis and Internal Obstructed Type
Therapeutic aim: Invigorates qi, enriches the blood and removes obstruction in the meridian channels
Prescription:
Bu yang hai wu decoction
Huang qi
milkvetch root
Gui wei
tail part of Chinese angelica root
Chis hao
red peony root
Tao ren
peach kernel
Hong hua
safflower
Di long
earthworm
Chuan xiong
Szechwan lovage root
Deficiency of Yin and Yang Type
Therapeutic aim: Nourishes yin and warms yang
Prescription:
Lu rong pill
Huang qi
milkvetch root
Ren shen
ginseng
Mai dong
dwarf lilyturf tuber
Wu wi zi
Chinese magnolia vine fruit
Xuan shen
figwort root
Shu di
processed rehmannia root
Yu ru
dogwood fruit
Lu rong
hairy antlers of young stag
Po gu zhi
malaytea scurfpea fruit
Ru cong rong
desert living cistanche
Di gu pi
Chinese wolfberry root-bark
Fu ling
Indian bread
Huai hiu xi
achyranthes root
Diabetes Mellitus : Prevention
Western Medicine
Our efforts in meeting the treatment goals are to prevent the onset or the progression of diabetic complications. These complications are categorized into microvascular and macrovascular problems. Microvascular complications result from poor glycemic control over a long period of time, and they are more commonly observed in patients with type 1 disease. According to the landmark study Diabetes Control and Complications Trial (DCCT) , intensive control with multiple insulin shots or insulin given via a pump into the body and self-blood glucose monitoring can reduce the onset of microvascular complications by about 60%.
Macrovascular complications may also present in patients with type 1 disease, but they are more common in patients with type 2 disease, who may have high blood pressure, high cholesterol / triglycerides, and / or overweight problems. The combination of these problems has been called a variety of names such as "Syndrome X," "Cardiac Dysmetabolic Syndrome," "Hyperinsulinemic Syndrome," and "Insulin Resistance Syndrome." Researchers believe that these metabolic problems stem from resistance to insulin and a state of hyperinsulinemia (when too much insulin is secreted and the cells are resistant to the available insulin). It is also believed that the syndrome as a whole is responsible for the macrovascular complications that are common in patients with type 2 disease. According to the United Kingdom Prospective Diabetes Study (UKPDS), achieving an HbA1c of 7% compared to 7.9% was associated with a 25% reduction of overall microvascular diseases. In addition, for every percentage point reduction in HbA1c achieved, there was a 25% decrease in diabetes-related mortality due to macrovascular complications, and an 18% reduction in combined fatal and nonfatal heart attacks.
Screening markers can help diagnosis
Because type 1 diabetes is of autoimmune nature, it is almost inconceivable to think it can be prevented. However, there are markers that can accurately identify first-degree relatives of those already diagnosed with the disease. Therefore, it is possible to screen these people by the HLA (genetic) type and potential interventions explored. In contrast, type 2 diabetes is caused by a variety of metabolic defects and it is possible that with healthy diet and behavior that its onset can be prevented or delayed. The prevalence of type 2 diabetes has increased significantly over the last 10 years or so. Some researches say this may be due to the growth of the aging population and people living longer. However, the incidence of diabetes has also been growing in the younger population, particularly in the teens. Factors responsible for this are probably many and include better diagnostic tools, and lower diagnostic criteria, as well as a tremendous increase in the prevalence of obesity. With better-designed public education programs targeted to the younger population regarding proper nutrition in diet, it is believed that the control of obesity will prevent the alarming increase of diabetes cases.
Public education programs
In addition to finding more effective ways to prevent or treat the symptoms and complications from diabetes, continuous research efforts in the areas of identifying physiological, genetic, and metabolic abnormalities associated with diabetes is necessary to conquer the disease and to avoid its worldwide increase. Although therapies for diabetes have been more specifically targeted to particular causative factors in recent years, focus on individual patients and personal treatment plans as well as intensive self-care should be emphasized in the next millennium. This will help control this disease, which has devastating implications in terms of morbidity, mortality, and healthcare dollars.
Chinese Medicine
Eat a balanced diet.
The Book of Plain Questions or Suwen (approx. 200 BC) says: "Cereal is the foundation of the basic diet, meat provides protein and fat which is very useful, fruits can promote the digestion of food, and vegetables provide suitable supplements." This ancient diet recommendation matches the modern day dietary management of diabetes, which is to eat a balanced diet with low sugar and fat intake.
Exercise regularly.
A nutritious diet and adequate exercise play important roles in diabetes. Daily exercise should be encouraged in order to promote the utilization of glucose (sugar) by the body tissues and decrease the body's insulin requirement.
Live a balanced life.
Long hours at work and a stressful and fast-paced environment can make people more susceptible to illness. As a result living a balanced life mixed with both work and pleasure can help the brain and body to stay healthy and may help to lessen the severity of the diabetes or prevent diabetes onset.
Be aware of family medical history and conditions that increase the risk of getting diabetes.
Individuals with a history of diabetes, high blood pressure and obesity in their family should be aware that these conditions could predispose them to getting diabetes. Additionally, individuals who already have risk factors such as high blood pressure and who are obese should regularly have their blood sugar level checked by their doctor to make sure they have not developed the disease.