甲狀腺功能亢進症 : Definition
Western Medicine
Hyperthyroidism, also referred to as thyrotoxicosis, is a condition that results from over-activity of the thyroid gland and consequent excess of circulating thyroid hormones in the body. Thyroid hormones have a direct effect on most organs and cells of the body. They essentially regulate metabolism and growth, and the symptoms of their excess are diverse.
The condition is common, especially in women, and usually occurs in those between the ages of 20 and 50 years. Hyperthyroidism is diagnosed in two per cent of women and is seen five to 10 times less frequently in men.
The thyroid gland consists of two lobes of soft glandular tissue joined by a narrow segment called the isthmus. The lobes lie either side of the trachea (windpipe) in the lower neck and in the normal thyroid measure up to 4 cm in length and weigh 15 to 20 g. They are well supplied with blood vessels.
Thyroid tissue is composed of vast quantities of sac-like follicles (small secretory cavities). These produce and store the thyroid hormones thyroxine (T4) and triiodothyronine (T3). The hormones circulate in the blood plasma largely bound to transport proteins. Production of T3 and T4 is controlled by the thyroid stimulating hormone (TSH), which is secreted by the pituitary gland in the brain, and is dependent on an adequate intake of iodine in the diet.
Normal thyroid hormone control
Chinese Medicine
Hyperthyroidism is a condition in which overproduction of thyroid hormone results in metabolic imbalance. The syndrome describes the signs and symptoms that result from an excess of circulating hormone. Graves' disease is the most common cause of hyperthyroidism. It is an autoimmune disease of the thyroid gland and presents with anxiety, a rapid heartbeat, sweating, increased appetite with weight loss, fine tremor of the extended hand and prominence of the eyes. The condition is more commonly found in women than men, in the ratio of 4:1, and is usually seen in the age group 20 to 40 years.
From a traditional Chinese medicine (TCM) viewpoint, hyperthyroidism is categorized as a "goiter." This is defined as a mass protruding over the area of the neck with localized redness; the mass may also be pendent and attached to the neck by a short stalk. This definition is similar to that of Western medicine.
TCM physicians believe that an improper diet and emotional problems, such as anxiety or anger, lead to stagnation of qi in the liver and spleen. This gives rise to accumulation of vital energy (qi) and phlegm in localized areas and facilitates the formation of a mass. The history of thyroid disease in TCM is long. It can be traced from as early as the Sui dynasty (581-618 AD) and is mentioned in the medical classic Zhubing Yuanhoulun (Treatise on the Causes and Symptoms of Diseases). Sun Simao (581-682 AD), one of the most influential physicians in the history of Chinese medicine, is renowned for his treatment of the disease. He recognized that hyperthyroidism arose from drinking water in certain mountain regions, and he also used the thyroid glands from deer and sheep, which have a high iodine content, to treat the disease.
Sun Simao (581-682 AD)
甲狀腺功能亢進症 : Causes
Western Medicine
There can be several causes for hyperthyroidism, but the most common are:
- Graves' disease
- toxic nodular goiter, and
- toxic adenoma.
- Graves' disease
Graves' disease, or primary toxic goiter, is the most common form of hyperthyroidism and accounts for 75 per cent of cases of thyrotoxicosis. It is an autoimmune disease in which antibodies produced by the immune system attach to specific sites on the thyroid gland and stimulate the gland to produce excess amounts of thyroid hormones. In the majority of patients this over-stimulation of the thyroid results in diffuse enlargement of the gland, a condition known as a goiter. The goiter can be two to three times the size of the normal gland and is accompanied by an increased blood flow. Diffuse goiters are only seen in Graves' disease and are more common in younger patients.
Enlarged thyroid gland in Graves' disease
Toxic nodular goiter
This form of hyperthyroidism occurs in 15 to 20 per cent of cases and tends to affect the older age group. Instead of the entire thyroid gland being enlarged, as in Graves' disease, abnormal growth occurs in multiple nodules. These nodules comprise thyroid cells that have lost their regulatory mechanism and secrete an excess of thyroid hormone. Thyroid nodules are found in four per cent of all adults, although individuals may be unaware of them, and again are more common in women.
Thyroid gland in toxic nodular goiter
Toxic adenoma
When nodular growth in the thyroid gland presents as a single lump, it is called a toxic adenoma and is commonly referred to as a "hot" nodule because of its hyperactivity. The condition accounts for less than five per cent of all cases of hyperthyroidism. The nodule is a benign (non-cancerous) tumor that secretes excess thyroid hormones and inhibits TSH secretion. This results in diminished function in the rest of the gland. Toxic adenoma tends to occur in women over the age of 40 years. The tumor is often more than 3 cm in size, but the symptoms of hyperthyroidism it generates are usually mild.
Thyroid gland in toxic adenoma
Other causes
Less common causes of hyperthyroidism include:
- Subacute thyroiditis. Painful inflammation of the thyroid gland by a virus induces a sudden release of thyroid hormones into the circulation.
- Postpartum thyroiditis. Temporary disturbances of thyroid function occur in five to 10 per cent of women within six months following childbirth. The condition is painless.
- Iodine-induced hyperthyroidism. Occasionally the administration of iodine in contrast media and the drug amiodarone (used for regulating heart rhythm) can result in hyperthyroidism. The disease is usually mild and self-limiting.
- Pituitary tumor. Very rarely a TSH-producing pituitary tumor (a malignant growth of the pituitary gland) increases secretion of thyroid hormones.
Chinese Medicine
Click here to see the causes of Hyperthyroidism from a TCM perspective
In identifying the causes of hyperthyroidism, most TCM physicians believe that when those individuals who are prone to a natural deficiency of yin encounter emotional problems, such as anxiety or anger, stagnation of liver-qi occurs. This generates fire evil and causes further drying up of the body's yin and blood. The liver then fails to perform its regulatory role for other organs, such as enhancing the digestive properties of the spleen.
If an individual is deficient in both liver-yin and kidney-yin, the body is then more likely to create phlegm evil. The phlegm evil obstructs the meridians causing an erratic qi circulation. When stagnant qi and phlegm evil collect in region of the neck, they give rise to goiter formation.
For a long time, TCM practitioners have believed that emotional and spiritual factors have a great influence on hyperthyroidism and result in a number of hyperthyroid-related symptoms:
- Over-stimulation by the seven modes of emotions leads to under-functioning of the liver and a failure in its regulation of the qi circulation. When too much qi is flushed up to the head, individuals become impulsive and irritable. They develop flushing of the face, blood-shot eyes, a bitter taste in the mouth, a dry throat, dizziness and vertigo.
- Emotional problems cause liver-qi stagnation and this generates fire evil. The fire evil damages the stomach, producing an increase in appetite and a persistent feeling of hunger.
- When qi flow in the spleen is disrupted, the digestive system is affected. Poor digestion and absorption result in weight loss and fatigue.
- Impaired function of the liver also affects the flush channel and the storage of blood. Amenorrhea (absence of periods) and irregular or scanty menstruation can follow.
- Deficiency of yin leads to hyperactivity of the prime minister-fire. This creates a condition where a virtual fire burns inside the kidneys causing nocturnal emission of semen and impotence.
- Deficiency of yin leads also to a failure of the kidneys to nourish the liver. Liver-yang becomes hyperactive and generates wind evil; this can cause hand tremor. Tremor or stiffening of the tongue may also occur. This abnormal state results mainly from endogenous wind evil and is also seen in alcoholism.
- Yin-deficiency in the heart and kidneys leads to palpitation, sweating, insomnia and nightmares.
- Yin-deficiency creates a virtual fire inside the body and individuals develop an aversion to heat. On examination, the tongue is generally red and the pulse is fine and rapid.
甲狀腺功能亢進症 : Symptoms
Western Medicine
The classical symptoms of thyrotoxicosis include:
- loss of weight
- palpitations
- breathlessness
- emotional lability (mood swings)
- increased sweating
- intolerance of heat, and
- goiter (diffuse enlargement of the thyroid gland).
Protrusion of the eyes is often seen in hypenthyroidism.
Other common symptoms associated with hyperthyroidism are fatigue, anxiety, agitation, mild tremor and muscle weakness. Itching and diarrhea can also be experienced and there can be hair and nail loss. Abnormal growth can occur in children and in premenopausal women, periods are sometimes light, infrequent or absent. Men may develop enlargement of the breasts.
In Graves' disease, the skin around the ankles occasionally thickens with the development of purplish-pink patches on the front of the lower leg. Many patients with Graves' disease have opthalmopathy, a condition in which the eyes appear to stare or bulge (exophthalmos). This is the result of swelling and increased pressure behind the eyeball, pushing the eye forward and causing the lids to pull back. The condition can cause irritation, ulceration and double or blurred vision.
The symptoms of hyperthyroidism often develop very gradually and patients may be unaware of them until they are quite pronounced. In older people, the classical symptoms may be absent and the patient just feels listless, anorexia, depressed and loses weight. The disease may present as heart failure in older patients.
Chinese Medicine
TCM practitioners will examine a sufferer and categorize symptoms under special syndrome groups known as "disharmony patterns." Certain disharmony patterns are present at different stages of a disorder. In hyperthyroid disease these can be classified into the following types:
Liver-qi stagnation, spleen deficiency and phlegm accumulation
Individuals present with depression, chest distress, pain in the area of the ribs, difficulty in swallowing, poor appetite and fullness after meals. They may sometimes experience nausea, weight loss and fatigue, diarrhea and protruding eyes. There is swelling in the thyroid region in the neck.
Deficiency in both qi and yin
Deficiency of these produces emaciation, fatigue and weakness. Sufferers develop an aversion to heat and experience sweating, palpitation, and soreness and weakness in the loin and knee regions. Again, there is swelling in the thyroid region in the neck.
Yin-deficiency and yang-hyperactivity
Individuals tend to be irritable and impulsive. They suffer from insomnia, palpitation, soreness in the loin region, general weakness, an aversion to heat, sweating, a flushed face and blood-shot eyes. They can develop a tremor in the fingers and an increased appetite, becoming easily hungry, thirsty and emaciated.
甲狀腺功能亢進症 : Diagnosis
Western Medicine
If hyperthyroidism is suspected, its diagnosis is easy to confirm. This is done by demonstrating the presence in the blood circulation of high concentrations of free thyroid hormones, T3 and T4.
Measurement of the level of thyroid stimulating hormone (TSH) in the blood is also carried out, as a low blood TSH level (resulting from negative feedback) will indicate that the thyroid gland is over-productive. This test also allows a differential diagnosis to be made between hyperthyroidism and pituitary tumor.
The measurement of the TSH level is invariably carried out in the elderly as physiologic changes and other illnesses can interfere with the interpretation of T3 and T4 levels.
The measurement of radioactive iodine or technetium uptake by the thyroid gland is also sometimes employed in the diagnosis of Graves' disease, especially if the symptoms peculiar to the disorder (diffuse goiter, discoloration of the lower leg and staring/bulging eyes) are not present. An injection of the mildly radioactive material is made into the blood stream and the thyroid gland is then scanned to determine how much material has been taken up. The radiation dose is extremely small and produces no side effects. Diagnostic radioactive iodine can also be given by mouth.
99mTechnetium scan of patient with Graves' disease showing diffuse uptake of isotope
Other biochemical abnormalities associated with hyperthyroidism include abnormal liver function tests, mildly raised blood levels of calcium and sugar in the urine.
Although it is fairly easy to make a clinical diagnosis of hyperthyroidism on signs and symptoms alone, it is essential to confirm the diagnosis in the laboratory. Thyroid function tests may need to be repeated more than once and treatment will depend on their results.
Chinese Medicine
Diagnosis in TCM places importance on determining the circumstances and manifestations of a disease through inquiry and symptom observation. Diagnosis is based on the traditional four examination techniques:
- Questioning The TCM practitioner will establish the medical history of both the patient and his family.
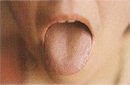
- Observation Examination of the physical features of the body, such as the face, tongue, hair, nails, sputum (mucus that is coughed up), and location of pain, all offer clues to the problem. The tongue is a particularly useful indicator of the functioning of the internal organs.
- Listening and smelling The smelling of sputum and breath and listening to the sounds produced by the chest offer additional clues to the patient's health.
- Touching Feeling the pulse is a cornerstone of TCM diagnosis and gives the practitioner much information about any bodily imbalance.
In hyperthyroidism, the procedures used in TCM to differentiate between disharmony patterns can be explained as follows:
Liver-qi stagnation, spleen deficiency and phlegm accumulation
When the liver fails to regulate the qi circulation, the spleen becomes damaged, digestion and absorption are affected, and phlegm evil is generated. Individuals present with liver symptoms, such as depression, discomfort in the chest and around the ribs, and protrusion of the eyes. Related digestive symptoms include poor appetite, fullness after meals or nausea, weight loss and fatigue.
On examination, the tongue is swollen, pink in color and indented on the margins. The tongue fur is white and greasy. The pulse is taut and fine, or fine and slippery.
Swollen, pink and indented tongue
Deficiency in both qi and yin
Stagnation of the liver-qi generates a lot of fire evil and this in turn depletes the qi and yin inside the body affecting other organs. For example, deficiency of heart-yin leads to palpitation, insomnia and irritability. When the spleen is deficient, insufficient protective-qi and nutrients are produced for the skin and muscles, and sweating, emaciation, fatigue and weakness occur.
On examination, the tongue is red with a coating of thin yellow fur. The pulse is fine and rapid.
Yin-deficiency and yang-hyperactivity
Stagnation of qi also results in liver-yang hyperactivity and a change in the emotional state. Heart-yin deficiency leads not only to palpitation and insomnia, but also to sweating and nightmares. When the stomach is damaged by liver-generated fire evil, individuals tend to have an increased appetite, become readily hungry and thin. The wind evil causes hand and finger tremor. Accumulation of virtual fire, which results from a relative excess of yang, causes an aversion to heat. The individual becomes thirsty and has a flushed face and blood-shot eyes.
On examination, the tongue is red. The pulse is taut and rapid, or fine and rapid.
Note: If a TCM practitioner suspects a serious problem that cannot be treated by Chinese medicine alone, he or she will recommend the individual to see a Western doctor for further follow-up.
甲狀腺功能亢進症 : Treatment
Western Medicine
Three forms of treatment are available for hyperthyroidism:
- drug therapy
- the use of radioactive iodine, and
- surgery.
The choice of treatment will depend on the cause of thyrotoxicosis and on its severity.
Drug therapy
Drug therapy includes the use of beta-blocking agents and antihthyroid drugs.
Beta blockers
Many of the symptoms of thyrotoxicosis, such as tremor, anxiety and palpitations, can be relieved very quickly by giving drugs known as beta blockers. These drugs (eg, propanolol) reduce stimulation of certain parts of the nervous system and decrease the activity of the heart. They do not have an effect on thyroid production, but in temporary forms of hyperthyroidism, such as thyroiditis, the use of beta blockers alone may be sufficient to control symptoms. Beta blockers are also very useful for preoperative preparation of patients for thyroid surgery.
Antithyroid drugs
Most patients with hyperthyroidism are given antithyroid drugs as initial therapy. The drugs commonly used are methimazole, carbimazole and propylthiouracil. They interfere with the ability of the thyroid gland to synthesize its hormones and are usually given in high doses until the thyroid gland functions normally (becomes euthyroid). This can take one to two months.
Patients with mild to moderate disease can usually then have the dose of antithyroid drug gradually reduced to the smallest that will maintain the euthyroid state. The maintenance dose will need to be continued for at least a year and possibly two. In some cases, therapy may need to be lifelong.
Sometimes the initial higher dose is maintained and supplemental thyroxine given. Some authorities consider that this regime provides a greater chance of lasting remission when the antithyroid drug is finally withdrawn, but the issue is controversial. Either way, therapy needs to be continued for at least one year to 18 months.
If therapy is withdrawn, frequent follow-up is important to make sure that remission is maintained. Relapses following withdrawal of therapy are common and occur in 50 per cent of patients, usually within two years.
Methimazole (available in the US) needs usually to be taken once daily only. Improvement in symptoms is seen in one to three weeks and control of symptoms is achieved in one to two months. Carbimazole (available in the UK) is rapidly and completely metabolized to methimazole in the body and it is this that is responsible for the clinical antithyroid activity. The dosage and use of both drugs is similar.
Both drugs can cause a skin rash. This occurs in about two per cent of cases. A disorder of white blood cells occurs much more rarely, but if a severe sore throat or mouth ulcers develop, patients should consult their doctors immediately.
Although methimazole and carbimazole are the drugs of choice in the treatment of hyperthyroidism, propylthiouracil is often prescribed instead if a patient develops a rash or is contemplating pregnancy. (Methimazole and carbimazole, taken before and during pregnancy, have been associated with abnormal nail growth in the fetus.)
Patients with severe hyperthyroidism or recurrent, relapsing disease may require to be treated with radioactive iodine or surgery.
Radioactive iodine
Radioactive iodine is iodine that has been bombarded with neutrons to create a different form of the element (an isotope). Radioactive isotopes are unstable and decay releasing a form of radiation. It is this principle that is used in radioactive iodine treatment.
The thyroid cells are the only cells in the body that are able to absorb iodine. By giving radioactive iodine, cells in the thyroid are damaged or destroyed and are unable to produce further thyroid hormone. There is little risk of radiation exposure to the rest of the body. A single dose of radioactive iodine, taken by mouth, is usually sufficient to provide permanent treatment. An endocrinologist will carefully calculate the dose before administration based on the results of the thyroid function tests. The drug is eliminated from the body within a few days, although it may be several weeks before the effect of the treatment is seen. During this time it is necessary to continue taking antithyroid drugs.
It is difficult to predict exactly the dose of radioactive iodine a patient needs to achieve the euthyroid state and sometimes after treatment the thyroid gland produces too little hormone (becomes hypothyroid). In this case, supplemental thyroid hormone in the form of thyroxine needs to be taken. Lifelong follow-up of thyroid function is needed for patients who receive radioactive iodine.
Radioactive iodine is commonly given in the following circumstances:
- In patients with Graves' disease unable to achieve lasting remission from disease with antithyroid drugs.
- As the treatment of choice for patients with toxic nodular goiter. (The incidence of hypothyroidism is much less common than after treatment for Graves' disease.)
- In the treatment of toxic adenoma. This also rarely results in hypothyroidism, as the shriveled cells around the nodule in the gland take up little or no radioactive iodine.
- Increasingly it is being considered as first-line therapy for adults with hyperthyroidism.
Radioactive iodine must not be given to children, or to women during pregnancy or breast-feeding.
Surgery
Surgery is mainly used for the treatment of hyperthyroidism that results from over-production of hormones in a section of the gland (rather than a diffuse over-activity) and it is reserved for a minority of patients with thyrotoxicosis.
However, some medical centers prefer its use to radioactive iodine in the treatment of recurrent Graves' disease. It is otherwise generally indicated in Graves' disease for those patients who:
- have very large goiters
- cannot tolerate antithyroid medicine
- refuse radioactive iodine treatment
- have opthalmopathy (staring/bulging eyes), or
- are young women and contemplating pregnancy.
The operation usually requires only a short stay in hospital. There is a small risk of injury during the procedure to structures lying adjacent to the gland, in particular to the nerve supply to the voice box. As with radioactive iodine treatment, the method can result in hypothyroidism if too much gland is removed, although the risk is less. Thyroid surgery should be undertaken only by an experienced specialist surgeon.
In nodular toxic goiter and toxic adenoma, surgery is commonly employed as an alternative to radioactive iodine treatment. The affected area of the gland or an entire lobe may be removed.
Finally, any nodular enlargement of the thyroid needs to be investigated, preferably by fine-needle aspiration biopsy and ultrasonography, to exclude the possibility of a malignant (cancerous) growth.
Chinese Medicine
The treatment of hyperthyroidism can be based either on syndrome differentiation or on symptoms.
Therapies based on TCM syndrome differentiation
Liver-qi stagnation, spleen deficiency and phlegm accumulation
Therapeutic aim: To relieve stagnation, reinforce the spleen, eliminate dampness and phlegm evils, soften and shrink the goiter.
Prescription: Decoction of Six Mild Drugs plus Xiaoyao Powder (modified)
| chai hu | hare's ear (root) |
| dang gui | Chinese angelica |
| bai shu | large head atractylodes root |
| fu ling | Indian bread |
| gan cao | liquorice root |
| zhi ban xia | pinellia tuber (processed) |
| chen pi | dried tangerine peel |
| xiang fu | nut-grass |
| bai shao | white peony root |
| bai ji li | caltrop |
| xia ku cao | self-heal |
| bai jie chi | white mustard |
| ze qi | sun spurge |
Deficiency in both qi and yin
Therapeutic aim: To benefit the qi and replenish the yin.
Prescription: Decoction of Six Drugs containing Rehmannia Rhizome plus Powder for Restoring Pulse Beat (modified)
| dang shen | pilose asiabell root |
| mai dong | lily-turf |
| wu wai zi | schisandra |
| sheng di | fresh rehmannia rhizome |
| shan yao | Chinese yam |
| shang yu rou | Asiatic cornelian cherry |
| bai shao | white peony root |
| huang qi | milk-vetch root |
| gou qi chi | Chinese wolfberry fruit |
| sheng mu li | fresh oyster shell |
| zhi shou wu | fleece flower root (processed) |
| sheng gan cao | fresh liquorice root |
Yin-deficiency and yang-hyperactivity
Therapeutic aim: To benefit the qi and replenish the yin, nourish the kidneys and depress the yang.
Prescription: Basic prescription
| huang qi | milk-vetch root |
| dang shen | pilose asiabell root |
| sheng di | fresh rehmannia root |
| gou qi chi | Chinese wolfberry fruit |
| zhi shou wu | fleece flower root (processed) |
| shan yao | Chinese yam |
| gui ban | tortoise shell |
| bai shao | white peony root |
| bie jia | turtle shell |
| xia ku cao | self-heal |
| xiang fu | nut-grass |
For individuals with severe goiter add:
| bai jie chi | white mustard |
For individuals with palpitation and insomnia add:
| yuan zhi | Chinese senega |
| ci shi | magnetite |
For individuals with severe hand tremor add:
| zhen zhu mu | nacre |
| gou teng | gambir vine |
For individuals with severe stomach-heat and excessive appetite add:
| tian hua fen | trichosanthes (root) |
| mai dong | lily-turf |
| yang shen | figwort root |
Therapies based on symptoms
Chinese medicine is also commonly used for symptom relief. In the treatment of hyperthyroid-related symptoms the following herbal medicines may be employed:
Profuse sweating:
| mu li san | oyster shell powder |
Or where sweating is extreme:
| huang qi | milk-vetch root |
| fu xiao mai | wheat (shriveled) |
Palpitation, nightmares and insomnia:
| suan zao ren | spine date seed |
| yuan zhi | Chinese senega |
| long gu | fossil bone |
| ye yiao teng | Chinese cornbind |
| zhen zhu mu | nacre |
Protruding eyes:
This is a difficult problem to treat. Relief can be obtained by removing heat from the liver and improving vision.
The main ingredients in the decoction include:
| zao xiu | paris |
| bai lian | ampelopsis |
| lou lu | fresh abalone shell |
| zhen zhu mu | nacre |
| shi hu | dendrobium |
| ju hua | chrysanthemum |
| gou qi chi | Chinese wolfberry |
| mi meng hua | buddleia |
| qian li guang | ragwort |
| gu jing cao | pipewort |
甲狀腺功能亢進症 : Prevention
Western Medicine
There are no known means of preventing the onset of hyperthyroidism.
For those individuals diagnosed with Graves' disease, it is important that medication be taken as directed and for as long as necessary to achieve the greatest chance of permanent remission from disease. Patient compliance in this is essential.
Although lack of iodine in the diet is associated with hypothyroidism, growth retardation and intellectual disability, it has been shown that in areas of low iodine intake there is an increased incidence of nodular toxic goiter, especially in elderly women. Only a few places in the world ensure adequate dietary iodine intake through natural foods (seaweed, kelp and other seafood) and most of the world's population relies on iodized salt for its source. In areas where there is no national supplementation program, it is important to ensure that supplemental iodine is taken, especially during pregnancy and in young children, to maintain a healthy thyroid.
Seaweed and kelp (often used in food processing) are rich in iodine
Although no other dietary precautions are necessary in hyperthyroidism, a well-balanced diet, adequate rest and moderate exercise will help maintain general good health and guard against symptoms of the disease being provoked or exacerbated.
Chinese Medicine
A diagnosis of hyperthyroidism requires proper precautions to be taken for its management.
The disease pattern can differ:
i. In one-third of cases, symptoms are alleviated after treatment.
ii. In a further third or more of cases, the disease shows periods of remission and relapse. It then becomes chronic and can persist for longer than 10 years.
iii. In rare cases, the disease becomes progressively worse after treatment and is associated with severe complications, which may be fatal.
Mental over-stimulation and stress should be avoided since these can affect the balance of yin in the body and liver's ability to function properly. Music therapy can be of benefit in regulating the emotions.
Music therapy
It is important to prevent the invasion of exogenous pathogens since they can damage internal organs like the liver. If invasion occurs, prompt therapeutic measures should be taken to counteract the effects.
Prevent the invasion of exogenous pathogens
Any medication should be taken or stopped only under medical advice.
Chinese medicines that are rich in iodine, like kelp and seaweed, should be used carefully and only with the supervision of a doctor.